Will Your Wishes Be Honored?
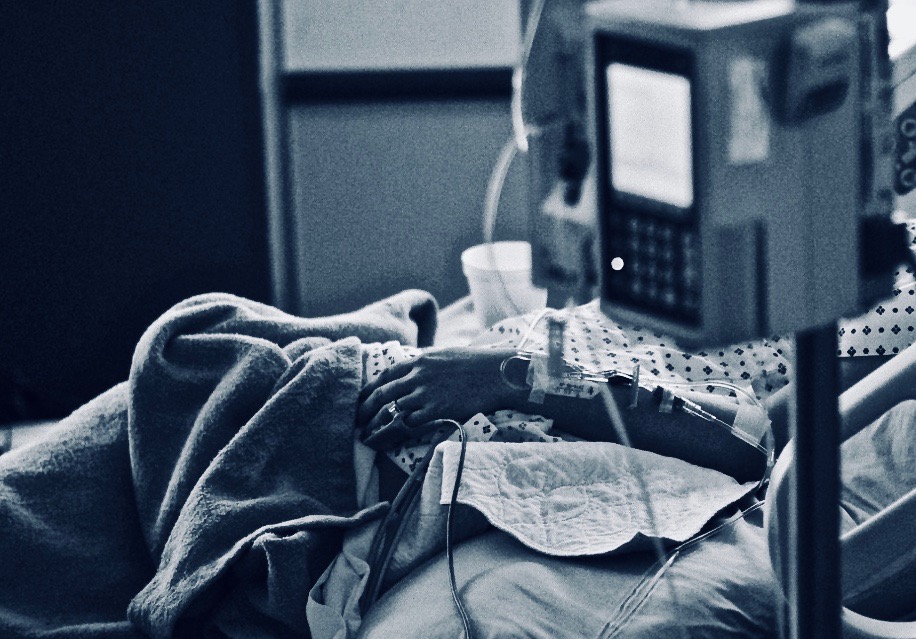
Some of the most frightening stories I hear are are from folks who are under the impression that they “have got that covered” when it comes to planning for care during serious illness or near the end of life. Unaware of how the medical system actually works, they are blissfully ignorant of the harms that may befall them and the anxiety their family and providers will face when the inevitable barriers go up and when questions asked are left unanswered. Then I start to hear, “If only someone had told me!” “If only someone had explained that back when….” “If we had known that we would have made a different decision!” Often by this point, it is too late. Too late to go back, too late to undo. By this point options are more limited.
When individuals fill out an advance healthcare directive in the absence of an informative discussion (as often happens when it is done as part of an estate planning process), they are usually unaware of how the medical system or their family members will interpret the language of the document when it is needed, when the owner of the document can no longer communicate their wishes, when they are at the bedside, when decisions need to be made. The terminology in the document is usually intentionally broad and vague. Leaving decisions, rightly, in the hands of the trusted healthcare proxy, the spokesperson. It is not currently common practice to engage the spokesperson in care planning conversations. At best, an individual might get some paperwork from a provider and told to fill it out at home and bring back to the provider’s office. But how often does that person take the time to educate their spokesperson? How often do they take time to update that information as their life and health status changes? I tell you: Not often, or not at all in most cases. Most individuals who find themselves in the position of making healthcare decisions for someone have had no preparation for that role. This creates confusion and stress.
Another situation I find scary is when people do try to plan and their plans are thwarted by a system or society that cannot accommodate their specific wishes either because of legal precedent, internal organizational policy, fear of reputation or diminished income. One situation that often occurs is when someone has determined in advance when or whether they would want assisted feeding or artificial nutrition as their health and independence wane. Flash forward a few years and that person may find themselves in a care facility that cannot accommodate that wish. The results can be devastating for the individual and the family. One recent story highlights the agonizing heartbreak this can bring and describes the ongoing controversy over assisted feeding and artificial nutrition in the setting of dementia.
Oregon recently passed legislation in hopes of clarifying some of these issues. In the legislation, they re-created a state-derived advance healthcare directive that allows individuals to make choices about “life support” and “tube feeding” when an individual is “close to death” or “permanently unconscious”. While this information may be helpful in some situations, in many it will be insufficient to guide care. Further, it does not address some the primary barriers that patients and families may face when making choices in the setting of dementia, other forms of cognitive and physical decline, or as the end of life approaches. I was not surprised by this, nor should you be. It is not possible in the context of ANY advance healthcare directive to consider or address the many complex and nuanced care situations or decisions someone may face at a future time.
What then is the answer? The safest route is informed planning! Get the information you need to make the care decisions you are most concerned about. Engage and discuss all aspects of your personal values and healthcare wishes with your chosen spokesperson. Make sure you back that up with an advance healthcare directive to give your chosen spokesperson the legal right to speak for you. Research your options for care and care settings, get the necessary information from medical experts to support a truly informed decision process. Keep your documents and conversations updated. Ask questions, get clear answers. An ounce of prevention is worth a pound of cure!
Get resources, make plans, communicate.
Guide for Conversations About Healthcare Decisions